
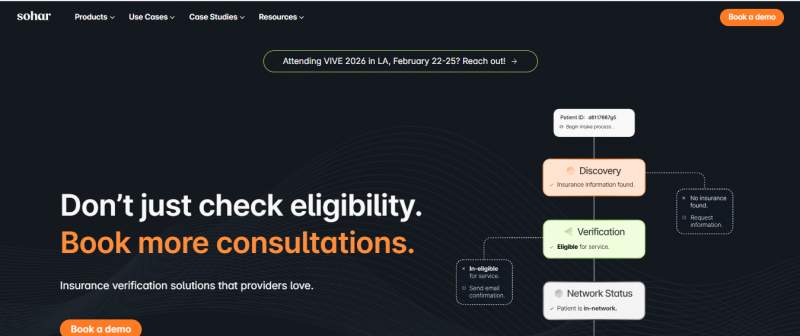
Sohar Health automates patient intake through insurance discovery, real-time eligibility checks, and network status determination. It identifies active insurance using first name, last name, date of birth, and state via the Discovery tool. Verification provides instant eligibility and benefits details across national and regional payers. Network Status confirms in-network relationships with customizable rules. These tools handle over 90% of verifications in under 30 seconds, reducing manual workflows in front-end revenue cycle management. The platform surfaces payer intelligence to correct member details and prevent claim denials.
99% accuracy insurance verification.
60% unknown coverage discovery.
Real-time VoB co-pays deductibles.
EHR Practice Management seamless integration.
Automates manual intake workflows.
API documentation gaps exist.
Accuracy issues certain payers.
Pricing yet to be updated!